Ultrasound4pets newsletter May 15
Newsletter May 2015
Firstly, many thanks to all of you who used our services in the first 4 months of Ultrasound4pets’ existence. We scanned over 300 animals including 70 echocardiography cases. Plus 40 odd dermatology patients. Phew!
Congenital defects
The number of portosystemic shunts and congenital heart defects out there is phenomenal. We have sent two pulmonic stenosis dogs off for balloon valvuloplasty and six shunts for surgical occlusion by one means or another. An unpublished retrospective survey by a UK cardiology diplomate looked at eventual outcome in puppies and kittens with murmurs where echocardiography was not initially performed for one reason or another -60% proved to have clinically significant heart defects. It’s probably better advice to just go ahead and get them scanned rather than wait and see.
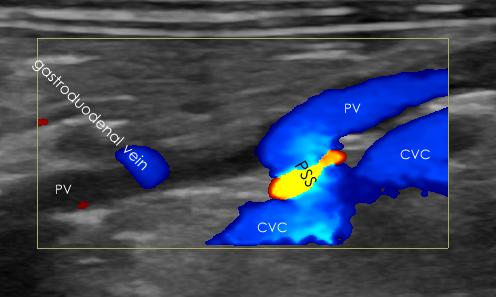
This is a classic spleno-caval shunt in a cat -the commonest configuration in both cats and dogs. Flow is diverting from the portal vein through the base of the splenic vein and thence via the shunt into the caudal vena cava. The portal vein cranial (left in this image) to the PSS is narrowed as blood flow has been diverted away.
EPIC study -implications for ultrasonography
This is a biggie! On 1st March this investigation into the use of pimobendan in dogs with degenerative mitral valve disease and cardiomegaly but WITHOUT signs of heart failure was terminated on account of mounting evidence that leaving patients in this category without pimobendan would be unjustifiable. All those dogs with murmurs really need scanning for evidence of left atrial dilation. Don’t wait until they develop CHF. In practical terms, I have been suggesting that all dogs over 5 years old with murmurs should be screened initially -depending on results we can then make a recommendation as to how often to repeat. That’s a lot of dogs. Time to buy shares in pimobendan manufacturers.
Ultrasonographic diagnosis of meniscal tears
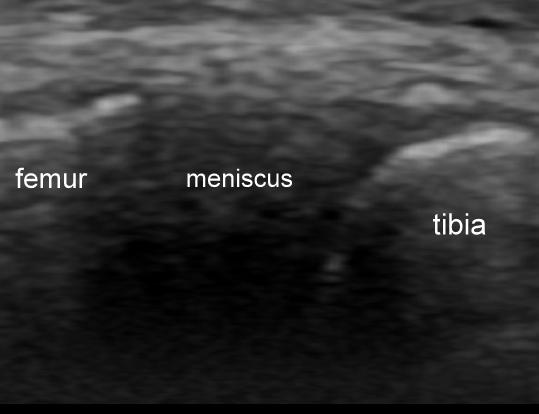
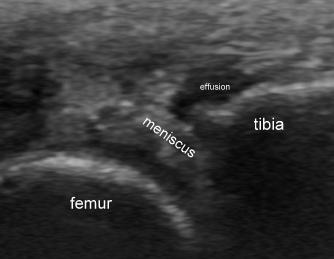
This is still an evolving area but very promising thus far. It’s relatively simple to scan the medial and lateral parts of the meniscii in dogs. Tears and/or degeneration are readily apparent in many dogs with stifle problems and, thus far, all cases which we have suspected ultrasonographically have been borne out at surgery. The best published paper (Arnault et al. VCOT 6/2009) found sensitivity and specificity of 82% and 93% respectively. This is especially useful now that it is not necessarily seen as obligatory to perform arthrotomy during surgery for cruciate rupture. It’s also very helpful when faced with a possible ‘late’ meniscal injury post-surgery.
Figures (from left to right): a healthy medial meniscus as seen from a caudo-medial viewpoint, a degenerated, frayed medial meniscus in the same plane of view and the excised meniscal flap from the same dog after excision.
Dilated cardiomyopathy or DCM-like heart disease in cats
There is intense debate over the cause and natural history of DCM-like conditions seen in cats without apparent taurine deficiency. Is this a discrete disease entity or the end-stage of other forms of cardiomyopathy? We have seen a few interesting candidate cases this month.
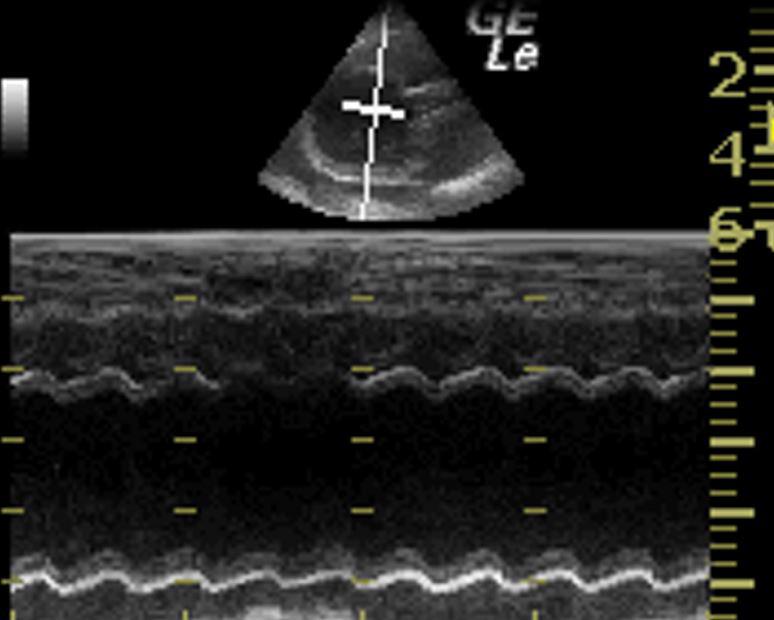
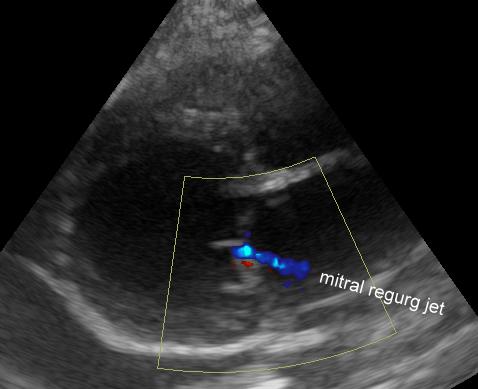
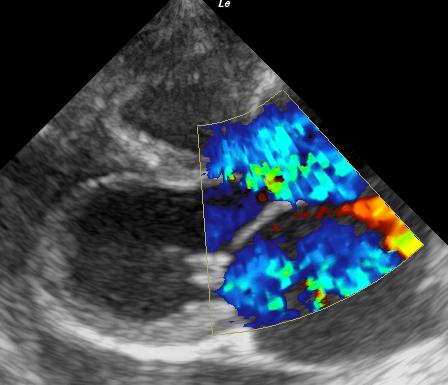
On the left is the M-mode from a Siamese with dramatic 4 chamber cardiomegaly and very poor systolic function. Her mitral regurgitation jet (centre) is a typical small, DCM -type affair due to dilation with resulting failure of leaflet apposition centrally. On the right is the heart of another cat -also with a very dilated heart and poor systolic function. But look at the mitral and tricuspid regurgitation jets and the extreme atrial dilation (relatively more than the ventricular dilation). I believe that this cat’s primary problem is A-V valve disease-either congenital or acquired (e.g. with endomyocardial fibrosis) -and we are seeing the end stage.
Immune-mediated pancreatitis in dogs?
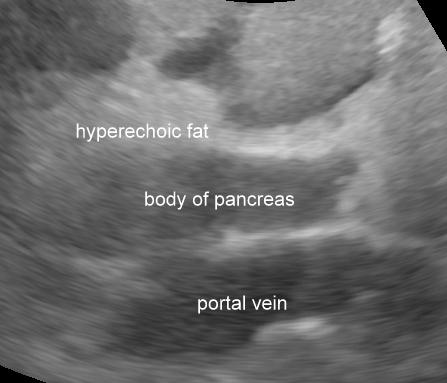
I-M pancreatitis is often suspected -particularly in Spaniels. We have recently seen a fascinating case with presumed I-M thrombocytopaenia who responded well to prednisolone but became inappetant with drooling and panting. On abdominal ultrasonography she has a convincingly hypoechoic pancreas.
….and, sure enough, her spec cPL was 600. So, what’s causing this? Really there is absoilutely no published evidence that glucocorticoids cause pancreatitis. She has had a few other medications -they are possible causes. However, the most interesting facet of this case is that,when we tapered down her prednisolone the cPLshot up to >2000. This situation is still evolving. My suspicion is that the pancreatitis is the result of an immune-mediated process related to the IM thrombocytopenia.
Talking of pancreatitis, I am commonly encountering situations where ultrasonographic findings do not concur with blood results for pancreatic lipase. There is a review this problem in the u4p blog at www.ultrasound4pets.co.uk -it’s not just me who suffers from this!
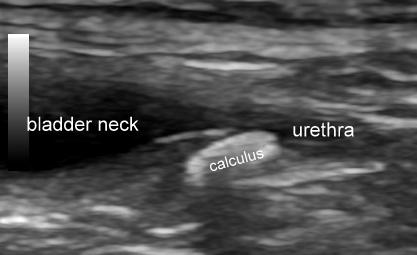
Ureteral calculi in cats
First described in 1991, ureteral calculi are now the ‘commonest cause of acute uraemia in cats’. This is a bit of a revelation! It’s well worth considering scanning those ‘kidney failure’ cats. This one washed out with fluid diuresis.
— . —-
Thanks again. Feel free to send me any interesting scan images you get yourselves
and see you soon. Roger