Successful treatment of eosinophilic ascites in a Labrador Retriever
The patient here is a 1 y.o. MN Labrador with a lifelong history of intermittent diarrhoea without specific diagnosis. He had been treated routinely with prophylactic moxidectin. Presenting complaint on this occasion was acute onset vomiting, diarrhoea, lethargy and ‘red eyes’ within 48 hrs of changing from chicken-based diet to lamb-based.
On physical examination he was in good bodily condition and generally, quiet but still responsive. He exhibited bilateral conjunctival erythema, T38.1, his abdomen was non-painful.
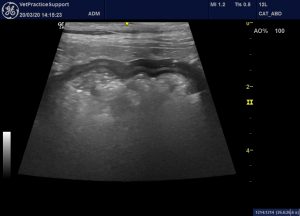
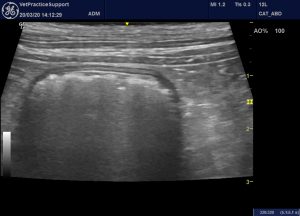
After symptomatic treatment, frequency of vomiting was reduced but he became more depressed and mildly hyperpnoeic. Routine haematology and biochemistry proved comprehensively unremarkable. Preliminary sonographic examination revealed small pleural and moderate abdominal effusions.
Systematic ultrasound report as follows:
thoracic ultrasound:
heart – subjectively unremarkable, all chambers and wall thicknesses in
proportion, systolic function adequate small pleural effusion, no pericardial
effusion
lungs unremarkable in part but there are scattered B lines and the pleura look thickened in places no mass lesions in visible parts
abdominal ultrasound:
moderate volume echogenic effusion
major vessels: unremarkable
abdominal fat: hyperechoic partly due to effusion
liver: size OK, shape OK, echogenicity diffusely a bit hyperechoic, vasculature unremarkable
portal vein: unremarkable
gallbladder and biliary tract: unremarkable except that gallbladder wall is diffusely moderately thickened
pancreas: unremarkable
stomach: diffuse mild wall thickening with hyperechoic mucosal change, lumen empty
duodenum: unremarkable
jejunum: unremarkable
Ileum: unremarkable
ICCJ: unremarkable
caecum: unremarkable
colon: contains a lot of gas and semi-liquid diarrhoea. Wall unremarkable.
spleen: unremarkable except for subtle patchiness
kidneys: unremarkable
adrenals: unremarkable, L gland 5.1mm diameter
ureters: unremarkable
bladder: unremarkable
proximal urethra: unremarkable
prostate: unremarkable
testes: unremarkable
jejunal, colic and other visceral lymph nodes: plump but not dramatic
sublumbar lymph nodes: unremarkable

Longitudinal plane view of the liver and cranial abdomen: there is a moderate volume effusion. The gallbladder wall is thickened.

Oblique view of the liver and gallbladder: hepatic parenchyma is diffusely but unevenly hyperechoic
Stomach wall: unremarkable

Jejunum: unremarkable
Colon: unremarkable
Abdominal fluid was obtained by abdominocentesis. Liver, spleen and bone marrow were aspirated with the following interpretation of findings:
Bone marrow: Eosinophilic hyperplasia.
Liver and spleen: A small amount of extra medullary haematopoesis.
Peritoneal effusion: Consistent with an exudate, eosinophil rich.
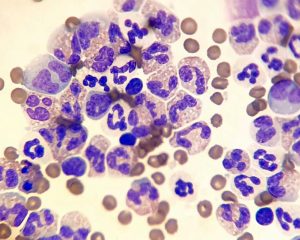
Eosinophil-dominated abdominal effusion (Photo credit: Corinne Ackroyd)
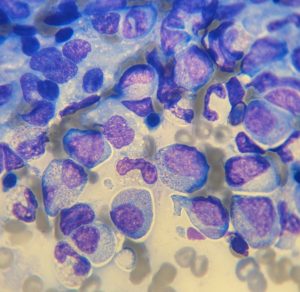
Bone marrow cytology
An Angiostrongylus antibody test proved negative.
With a provisional diagnosis of an eosinophilic disease process, a trial dose of injectable dexamethasone was administered. Within 24 hours the patient had recovered the normal joie de vivre of a 1 y.o. Labrador and was discharged with 1mg/Kg/day oral prednisolone and instructions to avoid further exposure to lamb. Prednisolone dose was tapered down and eventually discontinued after 6 weeks. He remains apparently healthy at the time of writing.
The option of endoscopic gut biopsies was declined.
An in vitro food allergen panel revealed raised levels of IgE against Lamb, Duck, Rabbit and Turkey. All other foodstuffs, including chicken, were negative.
Discussion:
Eosinophilic ascites has been described in a few human patients: in whom it appears to be associated with a subserosal form of eosinophilic gastroenteritis.
World J Gastrointest Surg. 2016 Sep 27; 8(9): 656–659.
Eosinophilic ascites: A diagnostic and therapeutic challenge
Shefali Agrawal, Sandeep Vohra, Sangeeta Rawat, and Vikas Kashyap
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5037340/
J Gastroenterol Hepatol 2012 Nov;27(11):1759.
Education and Imaging: Gastrointestinal: Eosinophilic Ascites
F Antonini 1, P Saltarelli, Giuseppe Frieri, Giovanni Latella
https://pubmed.ncbi.nlm.nih.gov/23106369/
Gastroenterology 2011 Apr;140(4):1149, 1364.
A Rare Cause of Ascites
Julien Jarry 1, Thierry Peycru, Manu Shekher
https://pubmed.ncbi.nlm.nih.gov/21352871/
Even in people this is a rare presentation. Affected patients often have a history of allergy in various manifestations (it’s interesting that the present canine patient exhibited acute conjunctivitis). Typically, as in the present canine case, onset of ascites is acute/subacute rather than chronic. In people, a peripheral eosinophilia is also characteristic.
Differential diagnosis includes parasitic disease; which seems unlikely here given this dog’s endoparasiticide history, and idiopathic hypereosinophilic syndrome: which usually follows a less benign course.
The human disease is also a highly steroid-responsive condition: typically with a tendency to relapse at intervals.
I can’t find any reports of similar cases in dogs. Circumstantial evidence supports the hypothesis that, in this patient, food allergy may have been the inciting cause.
Acknowledgment: thanks to the team at Yorkshire Vets, Thornbury who really did the work of fixing him.





