Spontaneous haemoabdomen in the cat
These images are from a 4 y.o. indoor DSH. Found acutely collapsed. No grounds to suspect trauma, no rodenticide access.
The thorax is unremarkable…except that the left atrium looked a little under-filled (long-axis end-systolic diameter 9mm).
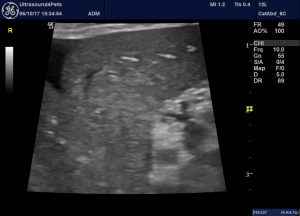
In the abdomen, there is a moderate volume effusion:
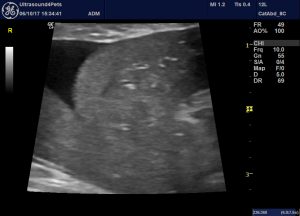
sagittal plane view showing liver and effusion
Although this image doesn’t show it, the effusion has a fine ‘granular’ echotexture to it.
The cava looks small:
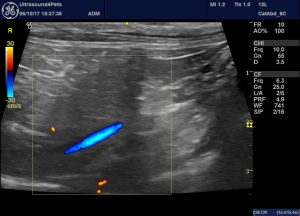
…a hint of hypovolaemia.
And the spleen is also, subjectively, small:
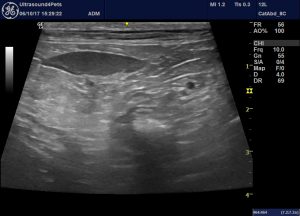
The abdominal fat is a little ‘bright’ but then an effusion of any kind will often do that.
However, there are no obvious mass lesions, no ruptures.
There’s an effusion -so we tapped it:

This looks a lot like blood. It doesn’t clot and cytology supports the diagnosis of hemoabdomen.
Coagulation parameters:

Reference range for feline APTT on this machine is up to 120 seconds.
Routine haematology revealed a moderate anaemia. Biochemistry showed an ALT 4 x top end of reference range.
Where does this leave us? We appear to have a ‘spontaneous’ haemoabdomen…i.e. one with no history or evidence of trauma.
Happily, there is a paper:
Spontaneous hemoperitoneum in cats: 65 cases (1994-2006).
https://www.ncbi.nlm.nih.gov/pubmed/20433398
The findings of this paper are interesting. In contrast to dogs, where the vast majority are undoubtedly neoplasia-related, fewer than half of the cats in this situation have malignancies (30/65). The spleen is the commonest affected site in cats with neoplasms (10/30).
The remaining majority were ultimately diagnosed with coagulopathies (8/35 -primary causes sepsis 4/8, rodenticide 2/8, pancreatitis 2/8), hepatic necrosis (8/35), ruptured bladder (5/35), hepatic rupture due to amyloidosis (4/35) and ruptured GI ulcers (3/35).
Overall, liver disease, neoplastic and non-neoplastic is the commonest source of spontaneous haemoabdomen (26/65 cases).
The pancreas, bladder and guts look unremarkable in our present patient. Although the abdominal fat is diffusely mildly hyperechoic there is no one focus of change. I often find it’s a useful exercise to sweep the probe relatively quickly across the abdomen and just gauge the distribution of any hyperechoic change.
Going back to the liver, however…..
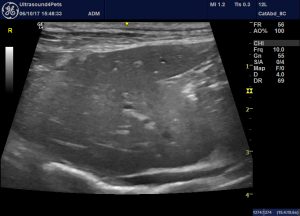
There is a hint of hyperechoic parenchymal change. And on closer inspection it’s quite convincing in some areas.
Obviously, we also have the fact that the ALT was very high (especially for a cat).
High APTT with normal PT is also potentially consistent with liver disease. This is a complicated area -summarised in this quote relating to the situation in human medicine:
‘Coagulopathy in liver disease has proven to be complex as it affects pro- and anticoagulant factors as well as pro- and antifibrinolytic components. The majority of coagulation tests are aimed at assessing the patient’s procoagulant capacity in isolation and do not reveal possible compensatory effects within the system. Furthermore, patients with liver disease are usually excluded from general guidelines on clinical decisions regarding transfusion before invasive procedures or surgery, in addition to guidelines on thrombotic risk and therefore thromboprophylaxis. Correct assessment of bleeding and thrombotic risk in cirrhotic patients should take into account several aspects, some of them outside the coagulation system itself as cirrhotic patients frequently bleed for non-coagulopathic reasons. From a haemostatic point of view, it is difficult to define criteria for managing these patients efficiently and safely and most decisions are based on clinical rather than scientific evidence.’
from:
Coagulopathy in liver disease: Lack of an assessment tool
Sadly, the prognosis for many of these cats is poor. Only 12% of Culp et al.’s cases made it out of the hospital. And our present patient continued to decline despite all efforts and was ultimately euthanased.
No conclusive diagnosis possible without histopath but I strongly suspect severe liver disease (necrosis, hepatitis or amyoidosis). Potential causes of necrosis include intoxication (e.g. fungi) and drugs (e.g. paracetamol, diazepam).





