Sonographic manifestations of bleeding disorders in dogs: including a case of apparent gastric purpura
It’s been a while since my erstwhile mentor Dr Bob O’Brien published this nice article:
Vet Radiol Ultrasound Jul-Aug 1998;39(4):354-6
Urinary bladder mural hemorrhage associated with systemic bleeding disorders in three dogs
R T O’Brien, E F Wood
https://pubmed.ncbi.nlm.nih.gov/9710141/
…and ultrasound technology has moved on a bit in the meantime. This is a recent case of the same phenomenon in a young Cocker Spaniel with profound thrombocytopaenia.
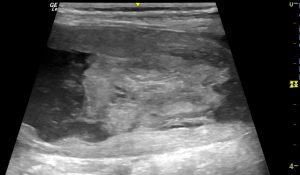
Longitudinal plane view of the bladder in a dog with presumed immune-mediated thrombocytopaenia and resulting haematuria.
The entire bladder wall has loss of normal layering and instead appears almost uniformly hyperechoic. The clot in the lumen is avascular on Doppler interrogation. This is a rather distinctive appearance. It’s important to say that these dogs may not necessarily have other physical signs of clotting disorders accompanying their lower urinary signs.

A slightly different angle to show local peritoneal effusion
Abdominal fat in the caudal abdomen is also locally hyperechoic; at least partly due to effusion.
It’s interesting to compare those changes with another thrombocytopaenic case. This 9 y.o. FN Dalmatian presented with haematemesis:

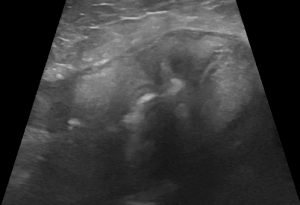
Sagittal plane view (transverse with respect to the long axis of the stomach) of the body of the stomach in a severely thombocytopaenic Dalmatian dog with acute onset haematemesis.
The stomach wall was diffusely, severely thickened but with preserved layering. However, there were some local, poorly defined, hypoechoic patches within the wall. The peri-gastric abdominal fat was markedly hyperechoic with that change being convincingly focussed on the stomach rather than on any other abdominal organ.

is could have been very challenging. However, the patient also exhibited evidence of clotting problems elsewhere which prompted rapid investigation of haematology and coagulation:


There had been no preceding signs to suggest a pre-existing gastropathy and there was no sonographic evidence of ulceration or stomach wall mass lesion. It seemed a reasonable hypothesis that intramural haemorrhage resulting from impaired clotting might be responsible. This would be akin to gastric purpura described in human patients:
Advances in Digestive Medicine (2017) 4, 39–40
A case with gastric purpura induced acute gastrointestinal hemorrhage
Tzu-Haw Chen, Chi-Yang Chang, Ching-Tai Lee
https://onlinelibrary.wiley.com/doi/pdf/10.1002/aid2.12039
Gastrointest Endosc 2009 Jul;70(1):167
Isolated gastric mucosal hemorrhages in idiopathic thrombocytopenic purpura
Shyam Dang 1, Muslim Atiq, Rahul Julka, Kevin W Olden, Farshad Aduli
https://pubmed.ncbi.nlm.nih.gov/19559840/
It’s interesting that, similar to the bladder haemorrhage case above, there’s clearly an appreciable reaction in the abdomen around the affected organ.
As a precaution, and following the recommendation of Dang et al….
‘The use of a proton pump inhibitor agent in a patient with GI bleeding often is a reflex action, but in this case, there was a sound physiologic reason: coagulation and fibrinolysis are strongly influenced by intragastric pH. At pH 5.4, platelet aggregation and plasma coagulation are virtually abolished; both improve with increasing alkalinity‘
…we treated with omeprazole in addition to immunosuppressive doses of dexamethasone/prednisolone. The patient made a rapid and full recovery without any evidence of ongoing gastropathy.
Finally, a coughing dog:
Bruce presented with acute severe cough and inspiratory stertor.

Transverse view of the mid-cervical trachea with carotid arteries on either side. The tracheal mucosa is thickened and irregular. The lumen contains hypoechoic material rather than air.
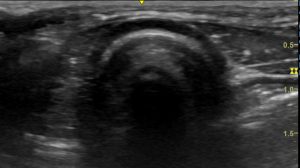
Transverse view of a healthy dog trachea for comparison.
There’s a marked hyperechoic reaction in the soft tissues around the trachea and the trachea is markedly abnormal. This is not typical even in severe upper respiratory infection. We were more suspicious of something along the lines of:
J Small Anim Pract 2006 Mar;47(3):161-4
Intramural tracheal haematoma causing acute respiratory obstruction in a dog
J J Pink
https://pubmed.ncbi.nlm.nih.gov/16512849/
J Small Anim Pract 1999 Dec;40(12):577-80
Acute tracheal obstruction associated with anticoagulant rodenticide intoxication in a dog
T L Blocker 1, B K Roberts
https://pubmed.ncbi.nlm.nih.gov/10664955/
J Vet Emerg Crit Care (San Antonio) 2018 Nov;28(6):573-578
Anticoagulant rodenticide toxicosis causing tracheal collapse in 4 small breed dogs
Amanda J Thomer 1, Kari A Santoro Beer
https://pubmed.ncbi.nlm.nih.gov/30294908/
…and, on checking, APTT proved to be very much prolonged (unreadably so). On further questioning there was an unequivocal possibility of exposure to rodenticide within the preceding few days.
Happily he recovered fairly uneventfully after a few days of vitamin K and mild sedation. Subsequent to our work up he did cough up some blood clots.
Cervical ultrasound has much to recommend it in this kind of situation. in a few seconds it’s possible to get a pretty good idea that there is a problem localised to the tracheal wall without any need for sedation, anaesthesia or advanced imaging. Coagulopathy would seem to be a possibility to be investigated at an early stage when faced with severe diffuse tracheal wall changes. Acute tracheal necrosis secondary to endotracheal intubation can cause similar but localised pathology.





