Pneumonia in dogs: gastrointestinal presenting signs
With the advent of lung ultrasound and the resulting great leap forward in our ability to diagnose bronchopneumonia relatively easily and with good specificity has opened a door on its true incidence and the spectrum of associated presenting signs. Notably, we now see affected dogs in which gastrointestinal signs are prominent. It’s hard to prove that the pneumonia isn’t the result of aspiration in a vomiting or regurgitating patient: obviously that is also a frequent scenario. However, circumstantial evidence is mounting and it’s backed up by case reports from human medicine,
A patient from this week: a 12 y.o. FN collie cross with no pre-existing medical conditions presenting with profound malaise and vomiting, fever and tachypnoea with a moderate neutrophilia. Blood biochemistry was unremarkable. There was no history of cough and, in the early stages, she didn’t cough in hospital either.
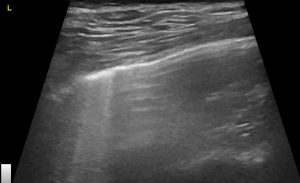
On lung ultrasound there was extensive consolidation of the right middle lung lobe with typical ‘shred’ or ‘fractal’ sign of pneumonia:

Frontal plane transthoracic view of the right middle lung lobe: showing ‘hepatization’, air bronchograms, peripheral b lines typical of bronchopneumonia.
The left lung lacked consolidation but showed increased B lines in some areas:
Left lung: given what’s happening in the right lung my assumption is that these B lines on the left (where consolidation was absent) may have been due to acute respiratory distress syndrome (ARDS) with ‘over-spill’ of inflammatory mediators from the right-sided pneumonia
Echocardiographic changes were limited to a decreased LV lumen: free wall ratio consistent with hypotension:
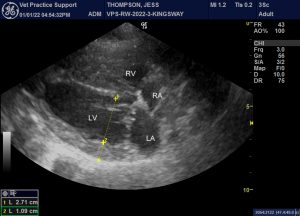
R long-axis 4 chamber view of the heart at end-diastole. LV lumen:free wall ratio should be at least 3.5:1. Lower than this, in the absence of LV outflow tract obstruction, implies either reduced filling (through, for example, hypotension or pulmonary arterial hypertension) or chronic systemic hypertension.
In the present case, obviously, pulmonary arterial hypertension (PAH) due to lung pathology is a significant possibility. However, 2D features of PAH were lacking and peak tricuspid regurgitation velocity was insufficiently fast to prove its presence.
Systemic blood pressure was measured at 70/45 (SAP/DAP): demonstrating marked hypotension.
Abdominal ultrasound showed no abnormalities of the gastrointestinal tract, adrenals or pancreas. The liver was diffusely hypoechoic:
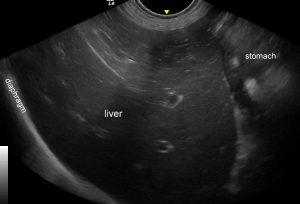
Longitudinal plane view of the liver from a point caudal to the xiphisternum in the ventral midline. Diffuse hypoechoic parenchyma is consistent with acute hepatopathy seen with systemic inflammatory response syndrome.

Diffuse thickening of the gallbladder wall. A non-specific finding but common in systemic inflammatory response (SIRS) scenarios.
This is all a bit anecdotal. We didn’t biopsy anything and it’s hard to prove that there weren’t other factors involved. However, circumstantially, I think it’s a reasonable working hypothesis that this dog, and other similar patients, develop gastrointestinal signs as part of a systemic inflammatory response syndrome / multiple organ dysfunction (SIRS/MODS) process. The gut is sensitive to metabolic changes in sepsis.
The same seems to happen in people:
BMC Infect Dis 20, 479 (2020).
Gastrointestinal symptoms in invasive pneumococcal disease: a cohort study.
Floeystad, H.K., Berild, J.D., Brandsaeter, B.J. et al.
https://bmcinfectdis.biomedcentral.com/articles/10.1186/s12879-020-05211-3
You can read the article but, to summarise, these authors reported that, in a large study over 16 years, 26% of their pneumonic patients exhibited gastrointestinal symptoms and that 11% of them had only gastrointestinal signs.
‘In this study, we found that more than a quarter of patients with [pneumococcal pneumonia] presented with GI symptoms at admission. These patients had a higher short-term mortality compared to patients without GI symptoms, despite being younger and having less comorbidities. The increased mortality became even more apparent when restricting the group to those who presented with GI symptoms only. Furthermore, we found that there was a delay in the initiation of adequate antibiotic treatment in the patients presenting with GI symptoms‘
It’s unclear whether increased mortality in patients with GI signs was due to delayed treatment or because GI signs reflect more serious systemic sequelae of pneumonia.
The implications of all this to our veterinary patients? It reinforces the need to include the lungs in point-of-care ultrasound (POCUS) examinations -and, indeed, that we should perform POCUS in as many sick patients as possible in order to avoid missing important diagnostic information.





