PDA with pulmonary hypertension in an adult dog: difficult decision-making
This is Cindy:

Cindy is a cutie. She is of indeterminate age but probably between 18months -3 years. She came from Romania originally and was then found to have a loud left basilar murmur with a thrill. At the time when this murmur was discovered she was asymptomatic. However, a few months later her owner reported reduced exercise tolerance.
On presentation for further investigation the murmur was loud, basal, ‘whooshy’ but not continuous -although the part of each cardiac cycle without murmur was very brief.
OK, so on echocardiography:

Right long axis 4 chamber view at end diastole
The right heart is unremarkable. But that left ventricle looks volume overloaded and the LV lumen:wall ratio is borderline high at 5:1.
There’s no significant mitral regurgitation on colour Doppler: this is already looking suspicious for a patent ductus.
The pulmonary artery is very wide:

right transverse view at the level of the main pulmonary artery
and colour Doppler demonstrates a lot of turbulence in the pulmonary artery:
https://youtu.be/vqWuPca0VX0?rel=0
Peak normograde systolic flow in the pulmonary artery is unremarkable: there is no evidence of pulmonic stenosis.
Furthermore, the turbulence can be seen to originate from a patent ductus in its characteristic location:

Right transverse view at the level of the main pulmonary artery showing the PDA
So far so straightforward. The remainder of the echocardiographic exam revealed no evidence of any other congenital defect.
And there is no current evidence of pulmonary oedema:

This is where is gets more complicated. From first diagnosis (and presumably from near birth) most dogs fall into one of two groups: having either left-to-right PDA flow or right-to-left PDA flow. The latter usually lack a murmur, have signs of caudal body hypoxia, polycythaemia and right ventricular hypertrophy: Cindy lacks these features.
Patent ductus arteriosi featuring left-to-right flow are usually subject to normal aortic-pulmonary artery pressure gradient. And since the pressure gradient is about 100mmHg or so, flow should have velocity about 5 m/s or so.
In Cindy’s case however, retrograde flow in the pulmonary artery and ductus have peak velocity < 2.0 m/s.
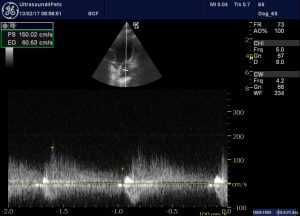
Right transverse view at the level of the main pulmonary artery with CW Doppler through the PDA
This implies increased right ventricular pressure consistent with developing pulmonary hypertension. Ideally this would be confirmed with tricuspid regurgitation velocity -but TR was lacking in her case.
We have to be careful that we are not just missing peak flow – jt can be surprisingly tricky to pinpoint within the PA. However, PW Doppler at a point within the ductus supports the contention that L > R flow is slower than expected.
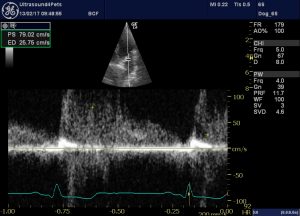
In fact, at the end of diastole there is a brief period of right-to-left flow -presumably explaining the break in the murmur.
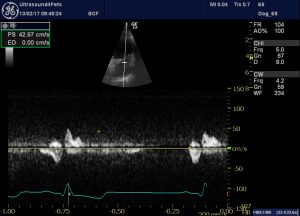
So it appears that Cindy falls into the mysterious minority of PDA cases which experience gradual reversal of flow associated with the development of pulmonary arterial hypertension.
The $90,000,000 question…..what are we going to do about it?
Surgical closure of fully reversed PDAs is clearly contraindicated. It is well established that this leads to acute right heart failure, massively reduced left heart venous return and thus output failure with death in late operative or immediate post-operative period.
However, Cindy is in a grey area. If we leave her un-operated the chances are that the flow will continue to reverse. We have the option to manage this medically with periodic phlebotomy if polcythaemia develops and to accept reduced exercise tolerance. Long term survival is unpredictable.
Or we can close the PDA and hope that haemodynamic changes are accommodated. There is some evidence from a handful of cases to support this option:
Successful closure of left-to-right patent ductus arteriosus in three dogs with concurrent pulmonary hypertension.
In fact these three dogs had more severe right heart failure than Cindy. Two had RV hypertrophy and the third actual right-sided congestive signs. And Cindy’s PDA flow remains clearly predominantly L > R -as evidenced by the initial 4 chamber view.
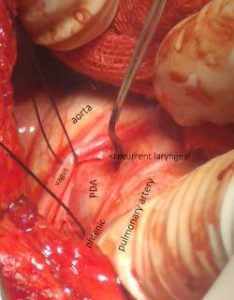
On this basis, and after a lot of discussion, her owners elected for surgical closure. Premedication included sildenafil 3mg/Kg p.o. in an attempt to promote pulmonary vasodilation. In the event, closure at thoracotomy
was uneventful although the hyperdynamic pulmonary artery presented more of a moving target area than usual.
She continues to do well at the time of writing.






I need help
My puppy is very small, what method did you use to close the PDA
Hi Cheryl, sorry probably you’ve got him/her fixed by now. Open chest surgery with ligation is feasible from about bodyweight 1Kg. Closure via intravascular occluder placement depends on the technology available to the surgeons. Some systems are limited to slightly larger pups.