More stem cell feedback: mesenchymal stem cells for cirrhosis
It’s always dangerous to read too much into a single case. However, this is potentially really exciting.
Bo, a female Giant Schnauzer, was only five years-old in 2017 when she became inappetent and developed a pronounced ascitic effusion. Serum biochemistry revealed mildly elevated liver enzymes and significantly supranormal post-prandial bile acids.
On ultrasonography, in addition to the effusion, her liver looked in bad shape: being small with diffuse hyperechoic change and numerous scattered hypoechoic nodules throughout.

There was no evidence of biliary tract disease, portosystemic shunting or other comorbidities.
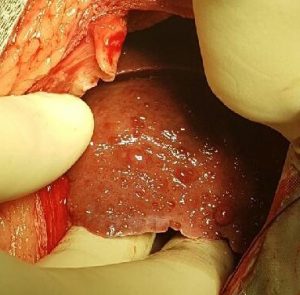
At laparotomy her liver also looked grossly abnormal with a lot of surface nodules:
Her histopathology report:
DIAGNOSIS Liver cirrhosis with dominance of the reparative (fibrosis) and regenerative process
HISTOLOGY Block A, three sections: The specimen reveals the presence of a marked disorganisation of the hepatic architecture with presence of a bridging fibrosis between periportal areas dissecting many small nodules composed of distorted hepatic cords, and degenerative and necrotic processes causing hepatocellular loss. Multifocal cholestasis is suspected. There are increased numbers of bile ducts in the periportal areas (bile duct hyperplasia, ductular reaction), with prominent vascular proliferation. Remaining hepatocytes often show vacuolar change. There are multifocal aggregates of lymphocytes and histiocytes. Kupffer cells and hepatocytes show brown fine granular pigmentation.
COMMENT The histology is diagnostic for the presence of liver cirrhosis.
Part of the reason for performing laparotomy for biopsy was to use the opportunity to harvest adipose (falciform fat) for mesenchymal stem cells. On the basis that we have no good evidence-based options for treating what we anticipated might well be cirrhosis it seemed a reasonable option. Some of the evidence to support the safety and potential efficacy of meschymal stem cells in canine liver disease has been listed in earlier blog posts.
Three weeks later we introduced 40,000,000 stem cells via ultrasound guided percutaneous injection into a splenic vein: facilitating their delivery to, and dispersal throughout, the liver.
Within six weeks the volume of ascites was subjectively but convincingly reduced to minimal levels. At the time of writing, 5 months post-diagnosis, she has regained apparently normal appetite and energy levels.
There’s limited good data on prognosis and survival times for dogs with cirrhosis. the best I can find is:
Diagnosis and prognosis of chronic hepatitis and cirrhosis in dogs
Sevelius, E.
Journal of Small Animal Practice (United Kingdom), 1995, v. 36(12) p. 521-528.
Amongst 33 patients with cirrhosis in this series mean survival was one week from diagnosis with just one living to two months. We hope to be able to gather a lot more follow up data from Bo. There are lots of caveats and one patient is no basis for any firm conclusions but it seemed to work for her.






Hì, how log did you inject the cells into the splenic vein?
what needle did you use?
thanks
Eleonora
Hi Eleonora,
Just injected them over the course of a few seconds using a 5cm 21G needle. To be honest I have now switched to simply injecting them into the liver parenchyma after reading some research which showed a higher integration rate after that route than via splenic/portal veins.
Thank you roger for sharing this with us here, it is really helpful.