Gastric ulceration in a dog with presumed hypoadrenocorticism
This is a bit of a heart-breaker really; it’s just that the images are dramatic.
The patient, a previously healthy young adult Chihuahua suffered acute onset malaise with occasional vomiting. Symptomatic treatment including NSAIDs at routine doses was administered. Subsequently she deteriorated abruptly becoming weak and recumbent with apparent abdominal pain. Routine haematology and biochemistry demonstrated mild anaemia, borderline hyponatraemia and borderline hyperuraemia.
On sonography the principal findings were increased cranial abdominal fat echogenicity and a dramatic diffuse thickening of the stomach wall -more pronounced towards the pylorus:

longitudinal view through the stomach to the right of midline
In transverse view, there is a deep ulcer in the pyloric antrum.
The remnants of the mucosa can be seen flapping at the margins. There are only a couple of millimeters of remaining stomach wall between lumen and abdominal cavity. The hyperechoic abdominal fat supports the idea that perforation may be imminent.
The adrenals are small:
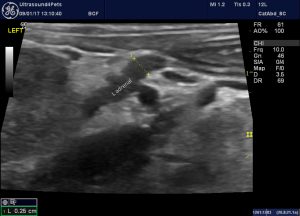
longitudinal plane view of the left adrenal
We know from:
Ultrasonographic evaluation of adrenal glands in dogs with primary hypoadrenocorticism or mimicking diseases.
That adrenal diameter <3.2mm is strongly suggestive of hypoadrenocorticism…..but this is a very small dog.
The pancreas, gallbladder and small intestine were largely unremarkable.
My main thoughts at this stage are:
- That ulcer looks alarming. Should we intervene surgically? However, this dog is looking very poorly, she’s recumbent and hypotensive despite IVFT: certainly an appreciable anaesthetic risk. Plus, as far as I can see, we have very little (like none) published evidence to guide us on the pros and cons of pre-emptive surgery.
- What is the primary disease process? gastric ulcers aren’t very common in young, healthy dogs. In fact almost every gastric ulcer I’ve ever seen in a dog has been due to chronic NSAID therapy. Hypoadrenocorticism, NSAID-induced ulceration or corrosive agent ingestion seem to be the most relevant possibilities.
- Immediate treatment. IVFT that’s a no-brainer. Sucralfate or aluminium hydroxide also not controversial. Intravenous PPI (pantoprazole is more available than omeprazole in the UK at this point in time) -seems sensible. Are we going to give glucocorticoids in view of the possibility of Addison’s but in the face of a deep gastric ulcer? -difficult call.
Sadly, events overtook us; she deteriorated and died before the basal cortisol could be run. The result eventually came back undetectably low -I think hypoadrenocorticism must be at least highly probable.
This is a somewhat abbreviated account of the case focusing on the ultrasonographic aspects.





