Cardiac manifestations of anaphylaxis in dogs
This is a difficult topic: anaphylaxis never comes with nice confirmatory histopathology, clinical pathology or advanced imaging. It’s a clinical diagnosis based on pattern recognition (acute onset and rapid remission, usually with prompt and full recovery, are important features). Partly for this reason I believe that it’s probably still widely under-diagnosed. At least, personally-speaking, I had never confidently diagnosed a case until about 5 years ago when a few key publications started appearing:
Anaphylaxis in dogs and cats.
Shmuel DL, Cortes Y.
J Vet Emerg Crit Care (San Antonio). 2013 Jul-Aug;23(4):377-94
https://pubmed.ncbi.nlm.nih.gov/23855441/
Sonographic changes of the gallbladder associated with anaphylaxis in dogs.
J Vet Emerg Crit Care (San Antonio). 2019 Mar;29(2):214-215
Comparison of clinical findings between dogs with suspected anaphylaxis and dogs with confirmed sepsis.
Walters AM, O’Brien MA, Selmic LE, McMichael MA.
J Am Vet Med Assoc. 2017 Sep 15;251(6):681-688
|
Sonographic features of anaphylaxis in dogs |
|
|
|
|
Obviously there are numerous potential causes of hypovolaemia but context is central: peracute cardiac under-filling in a dog who was running around a hour previously and has no major external fluid losses is likely to be due to anaphylaxis unless there is evidence of major organ pathology on systematic thoraco-abdominal ultrasound (GDV, colic torsion, haemothorax, haemoabdomen).
Neither is the ‘halo sign’ pathognomonic. However, the potential alternative causes (R CHF, other post-hepatic portal hypertension, cholecystitis, acute pancreatitis) are almost invariably less acute and less likely to be associated with severe cardiac under-filling.
As previously blogged, portal vein wall oedema may be a specific sign of anaphylaxis in dogs.
https://www.vetpracticesupport.com/ultrasonographic-features-of-anaphylaxis-in-the-dog/
Using these features, context of presentation and clinical pathology as the basis of presumptive diagnosis, we’ve come across a number of dogs in the last few years with particular cardiac manifestations of anaphylaxis.
Case 1: 11 y.o. MN Tibetan Terrier
This patient was outwardly fit and well albeit with a pre-existing systolic murmur and stage B2 mitral valve disease until he presented with acute profound lethargy, tachycardia of 240/minute and non-palpable femoral pulses. He was afebrile. Routine haematology and biochemistry revealed moderately elevated ALT and urea but were otherwise unremarkable.
On ultrasonography he exhibited marked left ventricular wall thickening in ratio to lumen diameter (hypertrophy or pseudohypertrophy) with no evidence of outflow tract obstruction.
His left atrium is enlarged due to MVD.
There’s no evidence of LVOT obstruction:
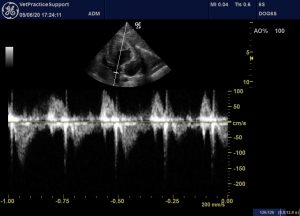
L apical subcostal view with CW Doppler through LVOT
And transmitral flow does not suggest L CHF (his lungs were also sonographically normal)
Left apical four-chamber view with PW Doppler of transmitral flow
ECG shows atrial fibrillation

Abdominal ultrasound showed typical anaphylaxis features:
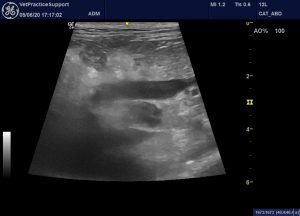
Hyperechoic peri-portal fat. Although the pancreatic body is also adjacent to this area, subjectively the change is focussed on the portal vein

Moderate, diffuse gallbladder wall thickening (presumed oedema): ‘halo sign’.

Right kidney: diffusely hyperechoic with reduced cortico-medullary distinction and multiple small cysts.
OK, so I have to admit that at this stage I was in two minds about all this. There are almost certainly multiple things going on. Atrial stretch due to MVD is a potential cause of AF. AF at this rate will significantly affect cardiac function and might be responsible for acute lethargy. He has raised urea and renal changes on sonography: systemic hypertension due to renal disease or even phaeochromocytoma is a potential cause of LV wall thickening. We were unable to measure blood pressure at initial presentation due to technical issues. Acute onset and portal vein/gallbladder changes suggest possible anaphylaxis but can’t be really confident.
We prescribed digoxin and diltiazem and gave a single injection of dexamethasone. He vomited after the first dose of antiarrhythmics and his owner didn’t give any more. By 48 hrs later he had returned to his normal self and was exercising and eating as normal.
ECG at 72 hours:

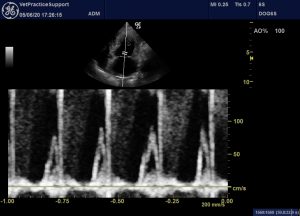
We’re back to sinus rhythm
And his heart looks much better filled:
Although his LV lumen:wall ratio remains slightly low for a dog with volume overload due to mitral valve disease and this degree of LA dilation.
His abdominal changes have resolved:

Subsequently he has gone on to resume life without external signs. Heart rate has been unremarkable whenever auscultated and sleeping respiratory rate is well within normal limits. Systolic blood pressure has been in the region 220-240 and is now managed with amlodipine.
Conclusions:
There’s strong circumstantial evidence that this was an episode of anaphylaxis superimposed upon CKD with systemic hypertension and B2 MVD. I find it difficult to imagine any alternative cause of transient profound hypovolaemia with concurrent portal vein and gallbladder wall oedema and prompt full recovery.
The AF is interesting. In dogs as in people the tendency for AF is multifactorial and LA dilation from whatever cause is a likely predisposing factor. However, transient AF is a reported sequel to anaphylaxis in people:
Am J Med 2017 Sep;130(9):1114-1116.
Atrial Fibrillation in Anaphylaxis
Patricia Rojas-Perez-Ezquerra 1, Blanca Noguerado-Mellado 2, Cristina Morales-Cabeza 2, Gabriela Zambrano Ibarra 2, Tomas Datino Romaniega
https://www.amjmed.com/article/S0002-9343(17)30592-2/abstract
Indeed these authors also state that ‘anaphylaxis can trigger any kind of arrhythmia.’ From a practical point of view they suggest that it is unlikely that glucocorticoid therapy would be contraindicated in an arrhythmic patient with potential anaphylaxis. The situation regarding the use of epinephrine in such a scenario is more open to debate.
The phenomenon of left ventricular pseudohypertrophy in anaphylaxis has been documented in affected people:
Anaesth Intensive Care 2019 May;47(3):295-299
Pseudohypertrophy of the left ventricle secondary to anaphylaxis: A case report
Christopher Ahg Wong, Sivasundari Arumugam
https://pubmed.ncbi.nlm.nih.gov/31172790/
Looking back at my previous posts on anaphylaxis I’m surprised that I hadn’t included this as a sonographic feature in dogs because it’s a central part of the phenomenon.
Case 2: 8 y.o. MN Golden Retriever
The patient, who had previously been completely healthy apart from a history of chronic, presumed allergic skin disease, presented with a history of peracute and sustained collapse.
On physical examination he was recumbent but conscious, responsive and afebrile. Femoral pulses were not palpable, heart rate was 88/min with regular rhythm. Routine haematology and biochemistry were unremarkable and cortisol response to ACTH administration was adequate.
Intravenous fluid therapy was administered and general attitude improved considerably to the point of becoming ambulant within a few hours. He was discharged from the clinic on the next day and sonography was performed two days later:
A small pericardial effusion was present:
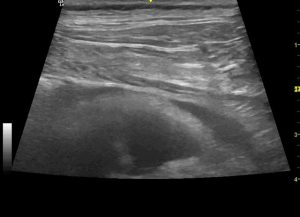
thoracic wall, pericardial effusion and section of heart
But the dominant cardiac finding was right ventricular dilation (LV internal diameter at end diastole: RV internal diameter = 1.7:1 where it would normally be about 3:1) and subjectively poor RV systolic function. There was no visible tricuspid regurgitation.
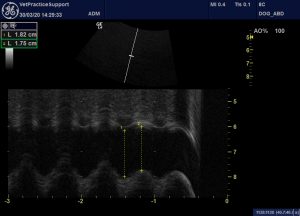
M mode assessment of the caudal vena cava at the level of the diaphragm. Diameter is reduced by only 4% on expiration (normally at least 50%)
Serum troponin was mildly elevated. The patient repsonded rapidly to initial fluid therapy and has gone on to resume healthy life as normal. On reassessment 3 weeks later echocardiographic findings and troponin had returned to normal.
Conclusions:
Again, circumstantial evidence, sonographic findings and lack of plausible alternatives favour a diagnosis of anaphylaxis.
Again, looking at what happens in people, a reversible cardiomyopathy associated with mild troponin elevations is well documented in association with anaphylaxis.
Int J Cardiol . 2008 Jul 21;127(3):e136-7.
Anaphylactic Shock-Associated Cardiomyopathy
Maximilian Hartmann, Christoph Bode, Andreas Zirlik
https://pubmed.ncbi.nlm.nih.gov/17651828/
J Investig Med High Impact Case Rep 2017 Jun 1;5(2)
Contrast Media-Induced Anaphylaxis Causing a Stress-Related Cardiomyopathy Post Percutaneous Coronary Intervention: Case Report
Rajeev Seecheran 1, Valmiki Seecheran 2, Sangeeta Persad 2, Sasha Lalla 3, Naveen Anand Seecheran
https://journals.sagepub.com/doi/full/10.1177/2324709617712735
The authors of the second paper classify this anaphylaxis-induced cardiomyopathy as a ‘stress-related cardiomyopathy’: a constellation of conditions (including Takotsubo cardiomyopathy) in which myocardial toxicity is believed to be due to catecholamines.
Ann Intensive Care. 2011; 1: 39.
Stress-related cardiomyopathies
Christian Richard
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3224539/
This second case is less conclusive. I wouldn’t like to claim that the diagnosis is firmly established; but it seems worth including the potential for anaphylaxis-induced, stress-related cardiomyopathy in this discussion.
Overall, the take home message is that anaphylaxis is a potentially many-faceted presentation. They often present to cardiology services and indeed they often do have cardiac abnormalities: such as arrhythmias, pseudohypertrophy and systolic dysfunction. Unless the abdomen is included in sonographic examination, it’s easy to miss the diagnosis.






Wow! I’m a cardiologist (https://www.premiermedicalhv.com/specialties/cardiology/), and my dog’s health problems brought me to this page. I’m blown away by the similarities between canine anaphylaxis and human anaphylaxis, especially the cardiac manifestations. Very interesting, and I’ll be sure to keep a closer eye on my pup from now on!
Thanks for your interest. Recognition of anaphylaxis in dogs is increasing dramatically…it’s a very gut based phenomenon in dogs often featuring acute portal hypertension, abdominal effusion and elevated liver enzymes.