Anaphylaxis, sepsis and pancreatitis
We are liking this very current article:.
Comparison of clinical findings between dogs with suspected anaphylaxis and dogs with confirmed sepsis.
- acute collapse was much commoner in anaphylaxis
- rectal temperatures tended to be higher in sepsis (although they ranged widely, no anaphylactic case was > 38.8)
- abdominal pain was commoner in septic dogs: presumably because the source of sepsis was often intra-abdominal.
- liver enzymes; see above
Obviously it’s also important to look for foci of potential sepsis such as GI perforations, abscesses and the like. Any effusions should be subjected to cytology looking for bacteria.
However, if you throw pancreatitis into the mix then things are becoming quite complex.

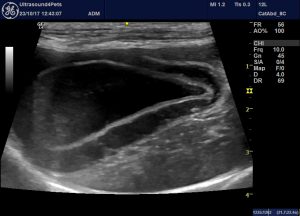
longitudinal plane view of the cranial thorax from lateral chest wall: pleural effusion is a surprisingly common finding in SIRS cases of all kinds. Not immediately what I would have expected with anaphylaxis until recent experiences.

Abdominal effusion
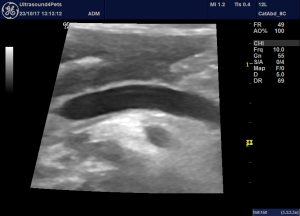
A so-called ‘halo sign’ consistent with gallbladder wall oedema

longitudinal plane view of the base of the right pancreatic lobe: there is subcapsular and interlobular oedema. Peripancreatic fat is somewhat hyperechoic compared to normal.

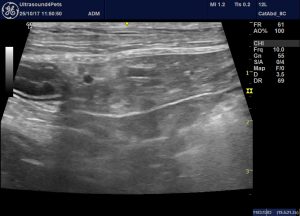
longitudinal plane view of the base of the right pancreas and adjacent duodenum

gallbladder
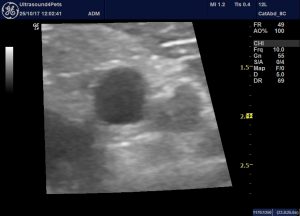
portal vein: transverse view





