Acute haemorrhagic diarrhoea syndrome (AHDS) in dogs: possible association with acute pancreatitis
AHDS (or HGE as it is probably more widely known) has long remained an enigmatic condition. Despite being common and serious, a definitive cause remained elusive. Cicrumstantial evidence supported the involvement of Clostridia but we lacked an explanation as to why only a few dogs develop signs when Clostridia are ubiquitous in gut flora…
….until now, possibly. This exciting new paper by Gohari et al. from 2015 describes an apparently convincing association between a newly-identified toxin and disease.
http://journals.plos.org/plosone/article?id=10.1371/journal.pone.0122684
From an ultrasonographic point of view AHDS is a common differential for many of the acute abdomens which we see. Obviously, it’s important to try to rule out GI obstruction and other concrete causes. However, there are specific findings which positively suggest acute enteritis.
Findings associated with canine parvovirus infection have been described:
https://www.ncbi.nlm.nih.gov/pubmed/20166398
These authors described diffuse mucosal speckling in the small intestine, reduced mucosal thickness, with some exhibiting intestinal corrugation and atony.
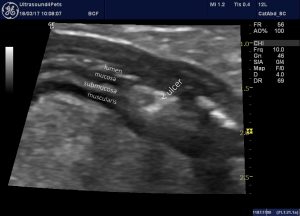
My impression is that dogs with severe presumed AHDS often have some loops of jejunum with diffusely hyperechoic (relative to normal) muscularis and/or mucosa. This contributing to a general loss of distinct layering:
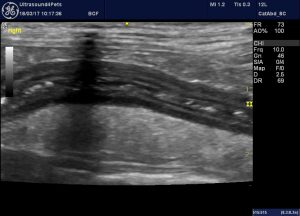
The severity of inflammation is reflected in the hyperechoic, inflamed appearance of abdominal fat surrounding the worst affected sections of gut.
This particular dog also exhibited areas which appeared ulcerated:
After recovering from the acute episode the patient continued to have waxing and waning inappetence with GI signs and eventually required a partial enterectomy to remove this section of necrotic jejunum.
These are findings compatible with histological descriptions of SI from fatally-affected dogs which feature mucosal necrosis. e.g.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4895553/
It’s useful to have a positive indication that there is diffuse intestinal wall pathology because these cases may take weeks to recover on occasion and, without reassurance from sonographic findings, clinicians are likely to feel obliged to continue pursuing alternative diagnoses (hypoadrenocorticism, pancreatitis, intussusception, chronic FB etc) and to come under pressure from owners who see a poorly dog and ‘no diagnosis’.
Gohari et al. also throw in a nice idea about the possible role of acute pancreatitis in AHDS.
‘In the light of the current advance in understanding the basis of canine hemorrhagic gastroenteritis, the well-recognized association of this disease with small breed dogs [14,15,58] may be explained by the increased incidence of pancreatitis in small rather than in large breed dogs [59], since pancreatitis will disrupt pancreatic trypsin production. By analogy, fatal type C C. perfringens enteritis has commonly been associated with trypsin inhibition by foods such as cassava, or by trypsin inhibitory factors in colostrum, with the consequence that CPB toxin produced in the small intestine is not destroyed by the proteolytic action of trypsin but rather initiates intestinal necrosis and cascading clostridial disease’
This makes a lot of sense to me. Below are images from a recent case of recurrent acute, hemorrhagic diarrhoea:

longitudinal plane view from the left flank showing descending (left) colon containing liquid diarrhoea

longitudinal plane view from the right flank showing the ileo-caeco-colic junction and the base of the caecum. The cacecal wall is markedly thickened.

Another section of inflamed caecum

longitudinal plane view from the left cranio-lateral abdominal wall: the left pancreas is swollen, hypoechoic and ringed by hyperechoic fat.
I guess, in the past, we might have hypothesized that the pancreatitis could be a sequel to severe enteritis (via SIRS etc etc).
This being a Mini Schnauzer, the discovery of apparent pancreatitis opens the way to chasing and controlling possible idiopathic hypertrigyceridaemia and maybe pancreatitis control could help reduce her AHDS episodes.





