A case of canine dysautonomia: sonographic findings, apparent response to steroids and discussion of the published literature

Murphy: he’s a 5 y.o. Cocker
Murphy initially presented with a two week history of vague malaise, occasional diarrhoea and abdominal discomfort followed by apparent constipation. Radiographs confirmed a very full colon and an enema was performed:

Radiography revealed a full colon and rectum. There’s no obvious evidence of megaoesophagus.
Within a few days, however, he had deteriorated further and now started vomiting/regurgitating. By this stage he was eating very little. Routine haematology and biochemistry proved unremarkable apart from a mild neutrophilia. Basal cortisol was >100.
On sonography:
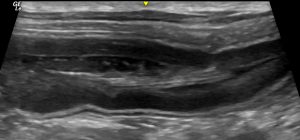
First things first, his lungs..
Lung: transverse view. That’s a classic ‘shred sign’ or ‘fractal sign’ of bronchopneumonia, Presumably due to aspiration.
This pneumonia was bilateral and likely severe enough in itself to contribute significantly to his degree of depression and anorexia.
Murphy’s cervical oesophagus was empty on sonography: with no evidence of abnormal retention of ingesta or saliva.
Neither pleural nor ascitic effusions were present. His liver was somewhat hypoechoic: that’s probably consistent with sepsis as a result of pneumonia.
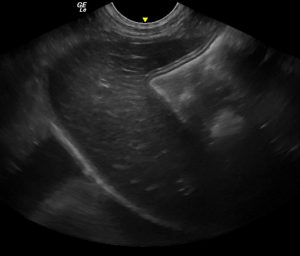
Longitudinal plane, mid-line view of the cranial abdomen. His liver is diffusely hypoechoic.
However, the dominant pattern of abdominal changes were gastrointestinal. His stomach was hugely dilated with liquid content and markedly hypomotile. This usually implies either functional or mechanical gastrointestinal obstruction.
However, most of his small intestine is pretty unremarkable.
Just the cranial duodenal flexure is somewhat dilated and also hypomotile:
In a transverse view, it was possible to see liquid/ingesta moving (in both directions) between pyloric antrum and duodenum: so no obstruction there. However, to complicate matters there was an apparent linear foreign body running through the pylorus:
Longitudinal plane view of the upper part of descending duodenum. That’s a grass blade in the lumen! Running through from the stomach.
These are really a sonographer’s nightmare. It’s very difficult to be sure whether that grass blade is just incidental; or whether it’s wedged enough, and abrasive enough to cause a gastritis/duodenitis.
His pancreas has some subtle hyperechoic marbling: but nothing dramatic enough to convincingly explain the severity of his overall illness. An in-house SNAP cPL proved negative.

Body of pancreas: oblique view from R (duodenum on R of image, liver to L of image)
Sometimes, with grass and such foreign material, all you can do is give it a bit of time and then reassess. So, this is his pylorus early the next day:
Obviously, the grass has moved on bit we still have the same degree of dilation and hypomotility.
His ileo-caeco-colic junction appears unremarkable: still no evidence of obstruction anywhere: and with his ileum being empty it seemed implausible that constipation in his colon could be causing pressure to back up all the way to his upper GI tract:
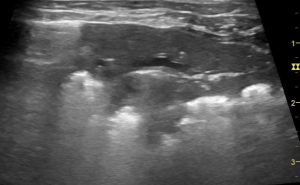
Gastric and small intestinal hypomotility without mechanical obstruction would be consistent with the ileus that often accompanies acute enteritis. It’s already a little suspicious, however, that he had been ill for a couple of weeks at that stage. Furthermore, rather than diarrhoea, his colon contains very solid, shadowing faeces:
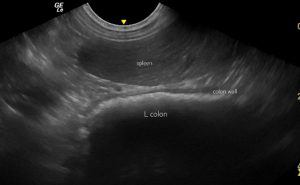
Left-sided longitudinal plane view with spleen (top of image) and descending colon below: that latter contains a lot of solid faeces consistent with history of constipation.
Interestingly, he had just been outside to toilet before this scan and yet his bladder is very full with no evidence of obstruction.
The possibility of leiomyositis was considered.
Jejunal muscularis thickness was as low as 0.2mm in some areas. This is low enough to fit with some published cases of leiomyositis.
At this stage, with no improvement despite symptomatic treatment including metoclopramide CRI, coamoxiclav for pneumonia and maropitant, the index of suspicion for dysautonomia, leiomyositis or gastrointestinal lymphoma had increased significantly. At laparotomy the absence of any gross extra-intestinal pathology was confirmed and multiple full-thickness biopsies were harvested from stomach and small intestine.
While waiting for histopathology, it became more obvious that Murphy was having issues of urine retention with some unproductive straining observed. Both pupils appeared inappropriately dilated with weak pupillary light reflexes. A Schirmer tear test yielded a markedly low result in his left eye (4mm) and borderline right eye (14mm).
Histopathology ultimately revealed no evidence of lymphoma or leiomyositis. But ‘in one of those gastric biopsies there is a small focal area in which neurons in one of the myenteric plexuses show very mild chromatolysis and the plexus a very mild infiltrate of lymphocytes‘. Whilst not pronounced enough to be, in itself, diagnostic this added to the evidence in favour of dysautonomia.
At this point, Murphy was transferred to a referral hospital for ongoing care. During the subsequent week he developed further evidence of dysautonomia including bilateral third eyelid prolapse and more convincing urine retention. During this period he was treated with oral bethanecol, lactulose and ocular lubricant. His vomiting/regurgitation resolved. However, he also acquired a unilateral facial paralysis -losing the ability to blink in the presence of intact (trigeminal) corneal sensation.
CT revealed only evidence of rhinitis. Brain/head MRI and CSF tap proved unremarkable.
Treatment with oral prednisolone 0.5mg/Kg sid was associated with a marked improvement in demeanour and appetite. He was able to leave hospital with continued owner assistance with bladder emptying and ongoing medication. Apart from a little weight loss he continues to do well at the time of writing two months after the initial ultrasound exam.
Conclusions:
I wanted to write up Murphy’s experience for several reasons.
1: canine dysautonomia is a rare condition, especially in the UK. Sonographic features in his case were broadly as one would expect but have not previously been documented in any detail to the best of my knowledge.
2: coexistence of a cranial nerve deficit with systemic dysautonomia is unusual and has implications for the possible pathogenesis of his problem.
3: it’s early days and impossible to know for sure on the basis of this case alone but, given that dysautonomia is generally associated with a poor prognosis (although occasional recoveries and partial recoveries are documented), it is at the very least interesting that he has appeared to benefit from glucocorticoid treatment.
Discussion:
Early reports of canine dysautonomia tend to involve uniformly high, often 100%, mortality:
J Vet Intern Med 1996 May-Jun;10(3):103-9
Dysautonomia in dogs: a retrospective study
R C Longshore 1, D P O’Brien, G C Johnson, A M Grooters, R A Kroll
https://onlinelibrary.wiley.com/doi/abs/10.1111/j.1939-1676.1996.tb02040.x?sid=nlm%3Apubmed
J Small Anim Pract 2007 Jun;48(6):346-52
Five cases of canine dysautonomia in England (2004 to 2006)
S J M Niessen 1, J Eastwood, J B A Smyth, G B Cherubini
https://pubmed.ncbi.nlm.nih.gov/17425697/
In some areas of the USA, there are local pockets of relatively high incidence.
The biggest UK case series of canine dysautonomia…
Dysautonomia in 53 cats and dogs: A retrospective review of clinical data and outcome
Katherine E Clarke, Stephanie M Sorrell, , Craig Breheny, Rosanne E Jepson, Sophie Adamantos, Elspeth
Milne, Danièlle. A Gunn-Moore
Vet Rec 2020 Dec 19;187(12):e
https://core.ac.uk/download/pdf/304334422.pdf
..includes one instance of two simultaneously affected dogs in the same household.
Unsurprisingly, presenting signs were very similar to Murphy’s case. Only 23% of dogs exhibited megaoesophagus. In this recent paper, there’s a glimmer of hope:
‘Of the 19 dogs included in this study, nine dogs survived to discharge (47%). Two cases were euthanised the week following discharge due to progressive clinical signs consistent with dysautonomia. One dog was euthanised seven months after discharge due to progressive clinical signs. One dog had resolution of clinical signs within two months of presentation and this case is still alive with no clinical signs 11 months following discharge. One dog had resolution of clinical signs within seven days of discharge but was lost to follow up. Long-term survival (greater than two years) was seen in three patients who are discussed below. Follow up information was not available for the remaining case.’
My reading of the article is that the long term survivor dogs didn’t have confirmatory histopathology. Thus the diagnosis of dysautonomia was one of strong presumption based on a clinical picture which ‘would be hard to attribute to any other single disease process, and had a clinical diagnosis made by exclusion of other causes‘. In this respect, Murphy is perhaps unique in having ante mortem histopathological evidence of dysautonomia and subsequent clinical recovery. His case provides some more concrete evidence to back up the hypothesis that some affected dogs do recover.
To the best of my knowledge, none of the published cases involve non-autonomic neurological signs. Murphy’s unilateral facial paralysis is a bit of a surprise. Dysautonomia (in the veterinary world) isn’t supposed to affect cranial nerves! Obviously, it’s possible that it could be coincidental (Cockers are over-represented in published case series of idiopathic facial paralysis)…although that seems to be stretching the bounds of coincidence.
Overwhelmingly, the dominant theory of causation in canine and feline dysautonomia is that of the unknown neurotoxin. I’ll admit to being a bit surprised that the literature of human dysautonomia paints a very different picture:
Here, the emphasis is on dysautonomia as a broad term encompassing autonomic nervous systemic dysfunction with a wide variety of causes…from autoimmune to paraneoplastic. You can read that page yourselves.
It’s not difficult to find human cases involving dysautonomia plus cranial nerve deficits:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8627825/
Obviously, in Murphy’s case there’s an interest in the idea of autoimmunity…since this would be a plausible explanation for multiple nervous system deficits and (possible) response to steroids. We don’t know anything like enough about his condition to draw any real conclusions; but, as a general concept there’s support:
https://www.ahajournals.org/doi/10.1161/JAHA.119.013602
https://www.frontiersin.org/articles/10.3389/fimmu.2021.702505/full
The USA picture fits the pattern of exposure to environmental factors as the commonest cause. In the UK, a sporadic pattern would fit possibility of auto-immunity.

At the time of writing, Murphy is hanging in there…having made it through the initial crisis. Currently he has full remission of GI signs and just a residual degree of urine retention.






Dear Roger
It is always fascinating to read your blog! It is a very interesting case indeed and well documented! Thank you for sharing with us
All the best from Transylvania, Romania
John
Hi Ionut! hope all is good with you there and thank you for your kind words. Keep in touch, Roger
Hello! Our golden retriever Runi has just been diagnosed with dysautonomia. Its hopeful to read about Murphy’s case.
Do you have any knowledge of his current condition and treatment since his recovery?
Any information is greatly appreciated!
Hi Jane, I’m not involved in his day to day care but I believe that he’s doing well…still on some treatment but not far off normal. Fingers crossed for Runi
Hi Jane. Chris & Freya here Murphys owner. Sorry to hear you’re going through a similar circumstance with your lovely golden Runi. I’m thankful to roger for his expertly written article to raise awareness and I’m glad it has helped with your situation with Runi so far.
*Update wise please note this is our experience and views as an owner*,
Murphy is doing great. Treatment wise his medication includes steroids once a day and myotoneine twice a day. His eyes have improved as well as his weight. His appetite seems to be even bigger than before and he has boundless energy since getting his strength back.
His only obvious symptom now is straining a little when he excretes however he can pass and empty himself compared to when he was first unwell. We aid this with laxatives.
Please persevere with Runi as I’m sure you are doing. There’s hope as there is no Formal diagnosis until post mortem and all indications when first diagnosed seem to be very morbid and upsetting. However we never thought we would be here 5/6 months later with Murphy and seeing him so happy.
Since the specialist input after his
Diagnosis. We have ourselves gone away and done our own research due to the complexity of this case and have considered rhinitus too.
Murphy will continue to be monitored and have check ups with the specialist for the long term but he seems happy within himself and experiencing no pain.
Please don’t hesitate to contact us again with any further questions. Kind regards