Pyelonephritis in cats and dogs: sonography and management
I feel that pyelonephritis is a bit of a neglected subject in small animal medicine. Since we don’t often do pyelocentesis, the diagnosis tends to be presumptive on the basis of UTI plus systemic signs. And when there are few confirmed cases then it’s hard to establish optimal treatment regimes.
Unless one does a lot of renal histopathology:
J Vet Intern Med. 2018 Jan;32(1):249-259. doi: 10.1111/jvim.14836. Epub 2017 Dec 2.
Pyelonephritis in Dogs: Retrospective Study of 47 Histologically Diagnosed Cases (2005-2015).
Bouillon J1, Snead E1, Caswell J2, Feng C3, Hélie P4, Lemetayer J2.
https://onlinelibrary.wiley.com/doi/full/10.1111/jvim.14836
In fact, this fabulous article is about the only decent primary source of hard facts out there!
Sonographic features of canine and feline pyelonephritis are sparingly described in the literature. Penninck and d’Anjou (Atlas of Small Animal Ultrasonography, 2nd Edition) list only diffuse hyperechogenicity, pyelectasia, distorted diverticulae and renal pelvis with hyperechoic rim as potential features.
The paper by Bouillon et al. gives a very similar list of sonographic findings. Adding presence of retroperitoneal fluid, increased or decreased renal size and hydroureter (which might be cause rather than effect obviously). The most important findings of these authors otherwise were:
- 75% of cases had comorbidities. Often predisposing or complicating factors.
- some cases with histopathologically confirmed acute and severe pyelonephritis were reported to have normal sonographic findings.
In human medicine, the majority of cases are reported to have no ultrasonographic changes.
https://radiopaedia.org/articles/acute-pyelonephritis-1
Apparently only about 25% have abnormal findings. These may include:
- particulate matter/debris in the collecting system
- reduced areas of cortical vascularity with power Doppler
- gas bubbles (emphysematous pyelonephritis)
- abnormal echogenicity of the renal parenchyma
- focal/segmental hypoechoic regions (in oedema) or hyperechoic regions (in haemorrhage)
mass-like change
Obviously it may well be that a lot of pyelonephritis goes undiagnosed in pets and that we see only more severe and/or more chronic cases.
In our experience the most striking changes in dogs and cats with pyelonephritis are not those described above. The ureters of affected patients are often abnormally obvious due to a combination of peri-ureteral hyperechoic retroperitoneal fat and thickened, hypoechoic ureteral walls. This hyperechoic change extends up to the renal peri-hilar fat.
The following patient is a 12 y.o. neutered male Labradoodle with a one week history of malaise, inappetence, hindlimb stiffness/lameness, occasional vomiting, pollakiuria, haematuria, polyuria/polydipsia, fever and mild neutrophilia.
His bladder, prostate and proximal urethra are unremarkable but for the presence of fine particulate matter:

But look at this left ureter!:
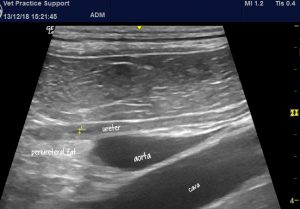
Longitudinal plane view of the mid-part of the left ureter and adjacent major vessels. The ureteral lumen is delineated by callipers.
That immediately jumps out as pathological. The combination of hyperechoic peri-ureteral fat and thick, hypoechoic ureteral walls imply a chronic ureteritis.

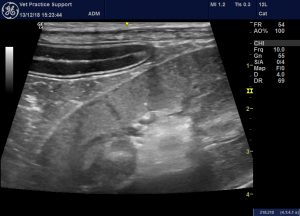
At the level of the kidney, the peri-hilar fat is bright and the renal medulla around the pelvis is hyperechoic (being almost isoechoic to the cortex):

transverse plane view of the left kidney. There is irregularity of the outline of the kidney with discrete hypoechoic, projecting ‘bulges’ (> <)
The discrete irregularities at the level of the capsule are presumed to represent renal capsular fibrosis or inflammation. Similar findings have been reported with pyelonephritis in other species.
The renal cortex is heterogeneous with an overall hyperechoic appearance contrasting with hypoechoic zones around blood vessels and below the capsule:
There is a mild lymphadenopathy of the sublumbar nodes: as often seen in UTIs.
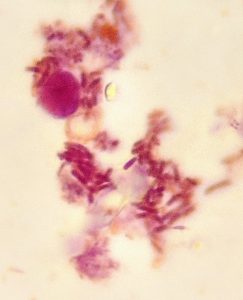
Urine sediment microscopy revealed vast numbers of intra-neutrophilic bacterial rods:
In really fine detail, the inner surface of the ureteral mucosa is delinated by patchy hyperechoic change. As here, at the ureter next to the papilla:
Peri-ureteral hyperechoic fat is also a feature in this area.
We would argue that this all adds up to a pretty convincing case for a diagnosis of pyelonephritis. The only other real differential for hyperechoic peri-ureteral fat is chronic or recurrent ureterolithiasis.
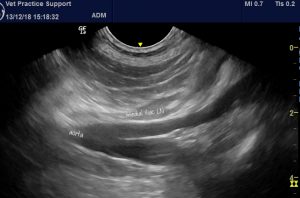
To prove this patient isn’t exceptional: this is a cat with severe chronic pyelonephritis exhibiting the same irregular thickening of the renal capsule and peri-nephric fluid accumulation.

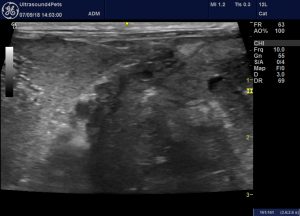
oblique view of part of the right kidney (right of image) and adjacent liver (left side of image). The renal capsule is thickened and irregular.
And a third case; also a cat, with a rather dramatic emphysematous pyelonephritis (hyperechoic gas bubbles):

…whose ureter is thickened, hypoechoic and contrasting with adjacent fat:

If the literature is light on the sonographic diagnosis of pyelonephritis, it’s positively deficient in evidence as to best treatment. Empirically, the long-standing recommendation from human medicine was that pyelonephritis should be treated with 6-8 weeks of appropriate antibiotics. This has found its way into the veterinary literature although, as far as I’m aware it’s not an evidence-based recommendation in either man, dog or cat.
In light of increasing resistance, short courses of treatment are preferred. In one clinical trial, a 7-day course of oral ciprofloxacin was shown to be a safe and successful treatment for acute pyelonephritis in women, including older women and those with more severe infection:
Ciprofloxacin for 7 days versus 14 days in women with acute pyelonephritis: a randomised, open-label and double-blind, placebo-controlled, non-inferiority trial.
Lancet. 2012; 380(9840):484-90 (ISSN: 1474-547X)
Sandberg T; Skoog G; Hermansson AB; Kahlmeter G; Kuylenstierna N; Lannergård A; Otto G; Settergren B; Ekman GS
https://www.ncbi.nlm.nih.gov/pubmed/22726802
There’s also not a whole lot of evidence as to best route although it seems to be agreed that prolonged intravenous antibiotics are not required.






Many thanks for the great images and fascinating explanation.