Iatrogenic overhydration: diagnostic nightmaresville
The inconvenient bottom line is that there is nothing intrinsic about the appearance of effusions or tissue oedema caused by fluid overload to distinguish them from those caused by congestive heart failure or any other pathological process. We have to infer the probable cause (or causes) from history, physical examination, clin path and imaging.
So, cardiogenic pulmonary oedema: we would expect a large left atrium, accelerated transmitral flow, shorter isovolumic relaxation time and evidence of (one or more of..) systolic dysfunction, valvular insufficiency or shunting. Well, the bad news is that large left atrium, fast E wave and short IVRT are also features of iatrogenic overhydration.
This is a lovely paper; one of my favourites:
J Vet Intern Med. 2007 Sep-Oct;21(5):1008-15.
The effect of hydration status on the echocardiographic measurements of normal cats.
Campbell FE1, Kittleson MD.
https://onlinelibrary.wiley.com/doi/abs/10.1111/j.1939-1676.2007.tb03057.x
The images are striking. It’s interesting that some of the cats developed murmurs as they became overhydrated.
It is true that the presence of apparent congestion plus LA^/E wave^/short IVFT without evidence of systolic dysfunction, valvular disease or shunting should make one look for the possibility of overhydration. It would be nice if that were a generally-applicable answer to to the problem. Unfortunately, a lot of hospitalised animals receiving intravenous fluids have medical conditions which might suppress systolic function. It can get very complicated…….
We recently saw a previously-healthy, middle-aged cat who presented with acute tachypnoea, hyperpnoea, anorexia, malaise and diffuse cutaneous erythema. He has a soft systolic murmur and a gallop. Routine haematology and biochemistry were unremarkable.

This is how his lungs look:
There is a ‘curtain’ of coalescing B lines and some patchy subpleural areas of flooding/consolidation/collapse. B lines indicate lung oedema in the broadest sense (i.e. not necessarily cardiogenic). He also has a small anechoic pleural effusion.
The oedema isn’t confined to his lungs. This is subcutaneous oedema of the inguinal area:

His cava at the level of the diaphragm is distended and doesn’t fluctuate in diameter with the respiratory cycle.

And the crunch issue, his heart:
That’s not easy….atria are a bit big. A 19mm LA (normal </= 16mm) is big enough to be compatible with left-sided congestive failure.
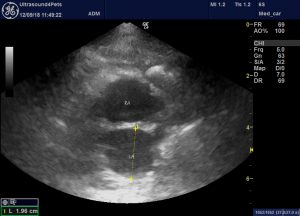
Although colour Doppler, indices of systolic function and wall thickness were unremarkable.
Abdominal ultrasound was otherwise unremarkable.
Oh, and by the time of scanning he’d been on IVFT for a couple of days (no diuretics given). Although respiratory signs apparently preceded fluid therapy.
On the basis that his valves and systolic function look OK I was suspicious that his lung and subcut oedema might be at least partly iatrogenic rather than cardiogenic. Hard to be sure though. Given that respiratory signs preceded IVFT it seems possible that there might be some acute primary lung pathology in addition to any secondary factors.
My no. 1 theory is that this may have been a respiratory virus (e.g. virulent systemic calici) with viral pneumonitis plus superimposed overhydration.
We opted to stop fluids, give frusemide and monitor respiratory rate closely and then taper down the frusemide. A week later he was completely back to normal and remains so to the time of writing.





