Heart and gut: interactions in disease
Yesterday I saw an elderly dog with recent onset anorexia, apparent abdominal discomfort, bloody diarrhoea, and a single episode of vomiting.
On examination this patient also turned out to have loud left- and right-sided systolic murmurs. And on echocardiography he exhibited findings consistent with left-sided congestive failure due to apparent mitral valve disease, secondary pulmonary hypertension and consequent right-sided failure.

Right transverse view of the left atrium and aorta: the atrium is greatly dilated. In scenarios of pulmonary hypertension due to primary lung disease the left heart is typically under-filled.

Tipped right long-axis view optimised for alignment with the main jet of tricuspid regurgitation: TR velocity of 3.5m/s implies a systolic pulmonary artery pressure of at least 60mmHg given that the right atrium and cava are large: convincing pulmonary arterial hypertension.
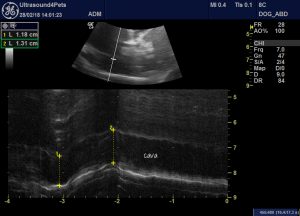
Long axis view from right abdominal wall of the cava as it crosses the diaphragm. In M mode there is minimal change in caval diameter through the respiratory cycle. In the absence of right heart failure the cava would normally collapse by at least 50% on inspiration.
On abdominal examination there is a moderate, anechoic, ascitic effusion: also consistent with right heart failure.

In parts of the jejunum there are areas of hyperechoic mucosal surface interface hyperechogenicity which suggest the possibility of ulceration:

Also, the liver is enlarged and diffusely hyperechoic with a coarse echotexture:

Biochemical changes included mild hypoalbuminaemia, elevated alkaline phosphatase, elevated urea with low normal creatinine and haematocrit within normal range.
We don’t really have enough information at this stage about this particular patient to know for sure what’s going on in the abdomen: but it’s an interesting exercise to speculate about whether heart failure may be contributing to abdominal sonographic changes and presenting signs. For this we have to go to the human medical literature:
Circulation. 2016 Apr 26;133(17):1696-703. doi: 10.1161/CIRCULATIONAHA.115.020894.
Gastrointestinal and Liver Issues in Heart Failure.
Sundaram V, Fang JC
This is a bit of an eye-opener to say the least! To list some highlights….
- In many human patients decompensation into failure is not associated with weight gain: fluid is, instead, being shifted from a reservoir in the splanchnic veins into general circulation, interstitial space and effusions. This is thought to be mediated by sympathetic drive.
- To quote the authors ‘These splanchnic hemodynamic changes may also be responsible for the abdominal discomfort, nausea, constipation, and diarrhoea common in advanced HF’.
- Heart failure is associated with an increase in circulating pro-inflammatory cytokines. The gut may be important in this process. Both hypoperfusion and wall oedema (i.e. both left-forward and right-congestive heart failure) cause increased gut permeability which may explain increased plasma endotoxin levels in heart failure patients.
- Heart failure is a potential cause and contributor to protein-losing enteropathy in people.
- Gut oedema may reduce absorbtion of orally-administered furosemide (but not torsemide).
- In people with right-sided failure venous congestion tends to lead to an ascites characterised by high protein content (compared to cirrhosis).
- Chronic hepatic venous congestion can actually cause progressive hepatopathy and ultimately cirrhosis.
- In 8% of hospitalised human heart failure patients abdominal pain attributed to hepatic congestion was the chief presenting sign.
- Jaundice, elevated alkaline phosphatase, hypoalbuminaemia and (less often) elevated transaminases are are common features of heart failure-induced hepatopathy.
Essentially it does indeed seem possible that heart failure might be an important factor in the presenting problems of our present patient. Or it could just be heart failure plus gastroenteritis….






Interesting case and good reference